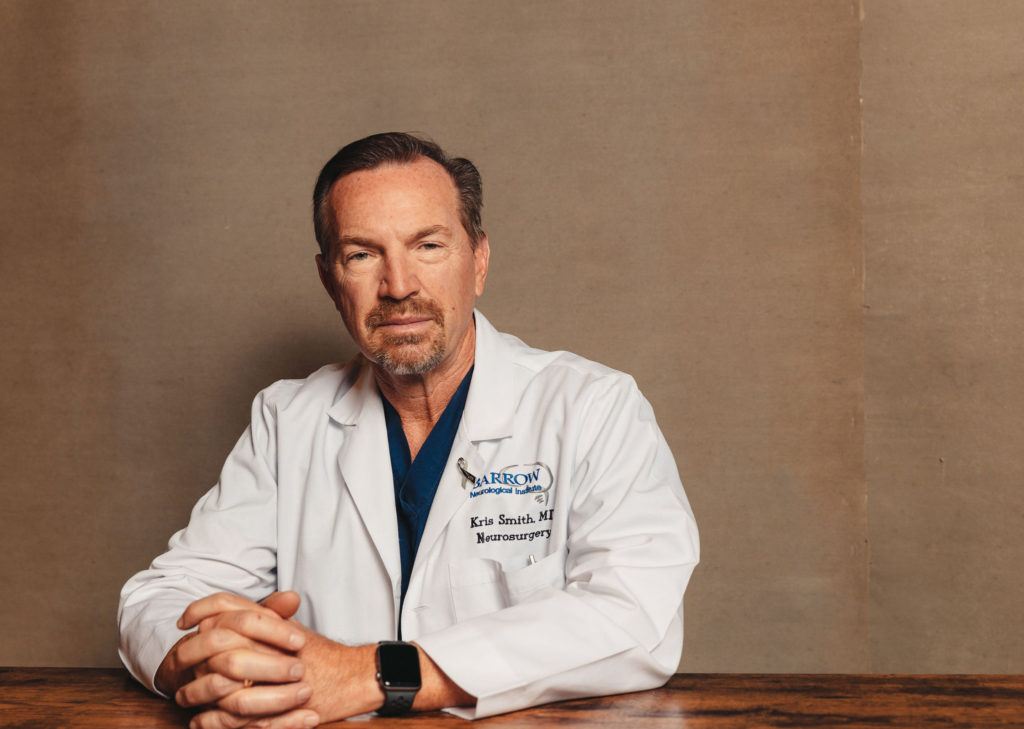
Kris Smith, MD
Neurosurgeon
Dr. Kris Smith is an experienced neurosurgeon who has treated brain and spinal tumors for decades. As a neurosurgical oncologist and investigator at the Ivy Brain Tumor Center, Dr. Smith aims to balance minimally-invasive techniques with surgical interventions to optimize patient outcomes.
Dr. Smith received his medical doctorate from the University of Nevada School of Medicine in Reno, Nevada, and completed his neurosurgery residency at Barrow Neurological Institute. Dr. Smith completed additional training in Gamma Knife radiosurgery at the University of Pittsburgh and at Karolinska Institute in Stockholm, Sweden. He completed a clinical fellowship in epilepsy surgery at the Cleveland Clinic.
As a longstanding brain tumor and epilepsy neurosurgeon, Dr. Smith has authored many peer-reviewed research studies and has held several leadership positions in professional societies such as the Arizona Neurosurgical Society and the Rocky Mountain Neurosurgical Society.
Dr. Smith has a unique understanding of the challenges his patients and their families face. When he was well into his career as a brain tumor surgeon, his father was diagnosed with a glioblastoma. After years of standard and experimental therapies, he unfortunately passed away. The experience enabled Dr. Smith to understand completely what his patients and their families endure.
“It has become my passion for trying to do things differently than they’ve always been done, to try to really understand the disease better, to try to treat the underlying cause of the disease. So, it’s really affected me,” he says.
Q&A with Dr. Smith
How did you get into neuro-oncology?
I felt drawn to improve the field of tumor neurosurgery, especially in gliomas. There was always this feeling of desperation and just giving up, that there wasn’t a good treatment for glioblastoma. And I found that to be very frustrating and an area that needed improvement. I became very interested in making the field better for these patients. And then, ironically, my father developed a glioblastoma and was treated here when I had already written a prospective clinical trial. We enrolled 30 patients in this very aggressive, upfront trial. He was patient number 14. It’s a bitter memory for me because he ultimately died, but there’s still one patient alive 16 years later. I just had a 16th birthday celebration with her.
What’s the best part of your job?
Well, there are a lot of things I love about being a neurosurgeon. Sometimes you get instant gratification when someone comes in with symptoms and they go home fixed, cured and happy. I just had an experience where a patient had a complicated recurrent tumor. After five years, it had grown back and was causing symptoms of progressive weakness, imbalance and dizziness. It was a very difficult one, but ultimately, after a 10-hour surgery, I saw him doing great the next day, up and walking around. During the battle, it was awful. But in the end, it was the best feeling you could have when he was up and around and moving. That’s the best part of my job.
The downside of my job is that it doesn’t happen to everybody. Despite all the things we try to do, these glioblastomas typically return. It’s a real passion of mine to improve treatment and patient outcomes. Not just that they live longer, but that they can live longer with a good quality of life, and that we don’t do anything to them that permanently damages their brain to cure their tumor. That’s been the holy grail.
Why is glioblastoma so challenging?
Well, unfortunately, a glioblastoma is not uncommon. It’s the most common malignant brain tumor in adults. In my opinion, finding a cure for glioblastoma is the most challenging problem in all of medicine. The unfortunate thing about glioblastoma is it doesn’t have just a single cell of origin. It doesn’t just start in one place. It’s a regional or global brain disease. And it eats the brain from the inside out, and that’s a really terrible thing. You can’t cure a glioblastoma by just surgically plucking out the tumor. We’ve learned a lot about everything this disease does to counteract our highly intelligent attempts at killing it off. But the more we learn, the more we understand the complexity of the disease.
What is the Phase 0 clinical trial approach?
With the Phase 0 approach, we are trying to capitalize on weaknesses that the tumor might have, and we learn about those weaknesses through molecular profiling. If a patient has a certain tumor with a certain type of biomolecular marker, it might show an area of weakness or a place we could target specifically.
New drugs come along that have been shown to be precise, and they attack a certain target. We screen the patients for a place of susceptibility or a target, a molecular-specific signature, and we match it to a drug that can attack it directly. We then give them the drug before surgery, for at least five days, as a very targeted approach. When we take the tumor out, we see if that targeted approach is working and if those molecules are actually attaching and starting to kill off the tumor. When it’s proven to be successful, the patient continues on that drug. If it doesn’t work, if it’s not attacking the tumor in the way we thought it would, then we don’t bother with that approach. We start somewhere else and do something different. It’s a very targeted, very specific, very scientific method of attacking the tumor and documenting a response.
Where do your research interests lie?
The concept people have heard of is precision medicine, and I coined the term precision metabolic therapy. Metabolic therapy means the patient’s metabolism is purposely altered into a ketogenic state to fight the brain tumor. There’s pretty good evidence in animal models that if we can get them into a ketogenic state, the chemotherapy and radiation therapy work much better. We’ve been able to cure 75 percent of the animals when they’re in ketosis with radiation and chemotherapy, whereas only 1 percent or less are cured without that state of ketosis. I’ve been trying to do this in our human patients, to get them to follow a ketogenic diet, but it turns out it’s not that easy, and it’s not a one-diet-fits-all approach. We look at the molecular profiling of the tumor. We’re trying to combine the patient’s nutrition genomics with their tumor genomics to find out if there’s a reason why they might have developed a tumor. We’re trying to look statistically at which patients with which genetic problems might have developed tumors in the first place and try to use that to treat the tumor. It’s a new and novel concept, but we have some anecdotal evidence that it is, in my opinion, the direction to go.
Click below to watch a video of Dr. Smith’s story.