Ivy Blog
70-Year-Old Soccer Star Scores Big Against Glioblastoma with Ivy’s Innovative Treatment
- December 10, 2024
- Ivy Center
- Posted in Patient Stories


The last six years have challenged Ann Rogers to the max, but she refuses to hit any wall without hurdling it. Her diagnosis of glioblastoma, the most sinister of brain tumors, is no different. She’s charging this opponent with the aggression of a world-class athlete, grateful for the game-changing expertise she receives at the Ivy Brain Tumor Center.
Resilient and optimistic by nature, Ann finds silver linings in every cloud. She was crushed by the loss of her daughter, Leilani, who died six years ago during pregnancy complications, yet she cherished the birth of her grandson, who brings so much joy to her extended family.

Her plans to retire on April Fool’s Day in 2020–from a successful career in software sales and education, IT consulting and training–collided with COVID-19, painting a retirement picture she hadn’t imagined. Six months into it, she received a breast cancer diagnosis, which had taken her sister at 44 years old.
On the bright side, Ann surmised, her cancer only required a lumpectomy and radiation, something she dismisses as merely a blip in life. She reimagined retirement and chose to focus only on what brought gratification: family first, followed by a passion for competitive soccer she’d cultivated surprisingly at age 40.
“Girls my age couldn’t play soccer when I was in school,” she says. “But I always loved it and have always been very active.” So when a colleague invited her to play in a co-ed team, she responded with the same curious, playful nature she leads her life: “Why not!”
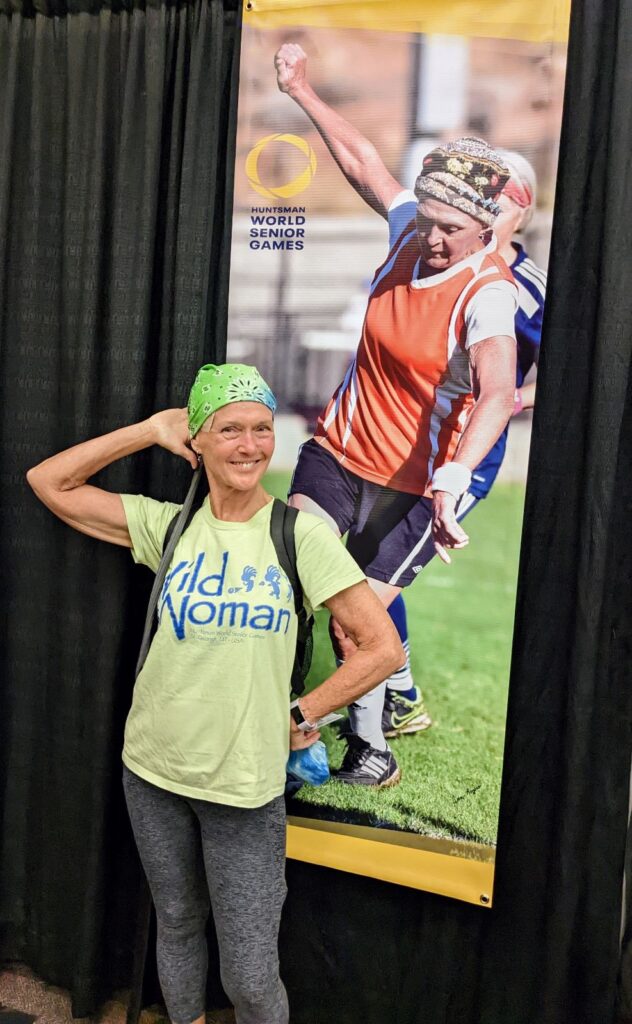
She’s played soccer ever since, joining a competitive women’s league that travels the country, celebrating wins and losses together, both on the field and in life. Like family, the sport and her teammates have helped her bounce back when times test her true grit. Like when she heard the word “glioblastoma” for the first time in a Denver emergency room on a Sunday evening in August 2021, just hours after wrapping up a soccer tournament and moments after finishing dinner with family.
“She started displaying significant expressive aphasia, and she just wasn’t making any sense,” recalls her son, Lyle. “So my sister rushed her to the ER. She thought it might be a stroke.”
Following CT and MRI scans, they received a diagnosis: A golf ball-sized glioblastoma tumor was growing on her left temporal lobe.
“I never had headaches or any other symptoms, plus I was in great shape and healthy,” says Ann. “I refused to believe it. I felt fine and said, ‘We’ll just battle this.’ I’m a warrior and I refuse to lose.”
Facing Facts About Glioblastoma
Glioblastoma statistics are daunting: Approximately 14,000 Americans receive a new diagnosis every year, 10,000 die from it, there is no cure, the median survival rate after diagnosis is eight to 16 months and, most alarmingly, that number has barely budged in the last two decades.
Glioblastoma tumors grow extremely fast and can double in size in a matter of weeks. Tumor characteristics vary widely from one patient to the next, making it difficult for clinicians to define effective treatment, especially given such a limited prognosis. While surgery to remove the tumor is the first line of defense, microscopic cells remain in patients’ brain tissue, allowing tumors to grow back … and they do, typically within a year or two.

Neuroresearch continues to advance, with new drugs constantly in development, though it can take years for FDA approval. Limited hospitals worldwide conduct clinical trials, complicating matters for patients to qualify and participate. Only one hospital in the U.S. offers the most cutting-edge research translated into real-time care: Barrow Neurological Institute, home to the Ivy Brain Tumor Center.
The Ivy Center operates the largest Phase 0 clinical trials program in the world. That means patients can access promising revolutionary treatments years before they are available as the standard of care, giving hope to those who have little time to wait.
When Standard of Care Isn’t Good Enough
Following her initial diagnosis, Ann underwent surgery to resect (remove) her tumor, followed by radiation and chemotherapy, the typical course for treating glioblastoma. She also started wearing an FDA-approved device known as Optune, which sends Tumor Treating Fields to tumor tissue to disrupt cell division and growth. In addition, she followed the regimen of quarterly MRIs to detect recurrence of the tumor, all under the guidance of her neurosurgeon and oncologist in Colorado.

Then, the waiting game began. Knowing it wasn’t a matter of “if” but “when” the tumor would return, Ann chose to play her own way, returning to soccer within six weeks and enjoying time with family.
Recalls Lyle: “That Christmas, she said, ‘You know, I’ve always wanted to see Europe.’ So we said, ‘Okay then, let’s do it, mom.’”

Ann was whisked away for several epic vacations–visiting England with Lyle and his wife, Charlotte; romping throughout France, Germany, Switzerland and Austria with Lyle, Charlotte and their daughter; and lastly, a tour of Ireland alongside her daughter, Alanna.
Settling back stateside, Ann pursued her passion for soccer and “doing things I love every day,” always seeking the best in life. “I just decided that whether it’s a month or 10 years, I’m going to make it the best that I can.”
Two years flew by, meaning she’d already lived beyond the median. She was just shy of the three-year milestone when her regular MRI sounded the siren: Her tumor was back on the hunt.
Knowing glioblastoma would always be lurking, Lyle was already mapping out a different line of attack. In the time since his mom’s first tumor resection, his wife Charlotte, an RN, had transitioned into a new role on the clinical research team at Chandler Regional Medical Center near their home in Arizona. The hospital is part of the CommonSpirit Health system that includes Barrow and Ivy, and it didn’t take long for Charlotte to learn about the significant advances they were making in brain tumor research and treatment.
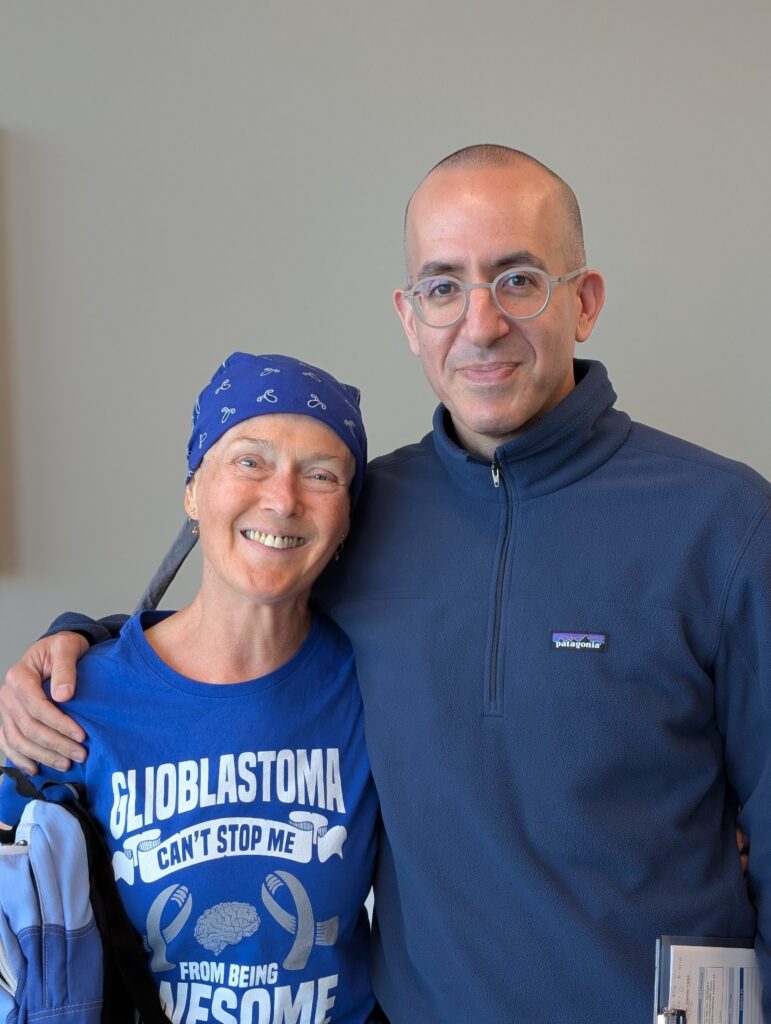
Lyle continued digging and uncovering facts about Phase 0 trials under the direction of Nader Sanai, MD, one of the most experienced and respected neurosurgeons in the world. “I knew when mom’s tumor returned, we wanted her surgeon to be Dr. Sanai,” says Lyle. He also hoped there’d be a clinical trial just right for his mom. Fortunately, it didn’t take too much to convince Ann, the warrior, to head to Phoenix.
Pushing for Hope, Relentlessly

Ann’s indomitable attitude mirrors that of Barrow and Ivy: Never give up on finding a cure for glioblastoma while seeking to extend life of the highest quality. When she first met Dr. Sanai, she was in awe, and both she and Lyle felt hugely assured by his comforting, confident presence.
Ann qualified for and enrolled in a Phase 0/1b clinical trial of AZD1390. The Phase 0 portion of the study confirmed the drug she took in the days leading up to her surgery penetrated her tumor at sufficient levels, so she graduated to an expansion phase that combines therapeutic dosing of AZD1390 with standard-of-care radiation.

The last couple of months have been some of Ann’s biggest and best: Already a grandmother of 6, she turned 70, celebrating with a family ziplining adventure, and she gleefully welcomed her first great-grandson into her arms.
She also underwent surgery to remove as much of the tumor as possible, followed by radiation and chemotherapy. As part of the study, Ann is also participating in the Ivy Center’s liquid biopsy program, which is the most advanced technique available to track her tumor and define the course of treatment that allows her to live to the fullest.
“Our strategy is the first of its kind and allows us to follow tumor changes month to month, even when these changes remain undetectable on brain imaging,” says Dr. Sanai. “Ann’s participation in the program can potentially benefit herself and many glioblastoma patients in the future.”
Ann is abundantly grateful to have caregivers–including Dr. Sanai, her radiation oncologist Dr. Igor Barani, neuro-oncologist Dr. Kelly Braun and neuro-nurses at Barrow–rooting her on every step and kick of the way, especially as she prepares to return to soccer in January.
“Everyone has been wonderful, very kind, very knowledgeable,” says Ann through tears. “I’m so thankful and respect them so much. They’re very passionate about doing everything they can.
“And, you know, I fully intend to be successful for them because we all want to win, right?”

Liquid Biopsy: The Most Advanced Technique for Tracking and Treating Glioblastoma
The Ivy Brain Tumor Center’s recent launch of the Liquid Biopsy Program might be a game-changer for patients with glioblastoma. The program gives doctors real-time insights into how a patient’s brain tumor responds to experimental treatment.
Following glioblastoma diagnosis, patients typically undergo surgery to remove the tumor, then receive radiation and chemotherapy to remove any remaining cancer cells, following up with MRIs every three months to see if the tumor returns. But, an MRI can’t detect as much information about the patient’s tumor cells as quickly as a liquid biopsy.
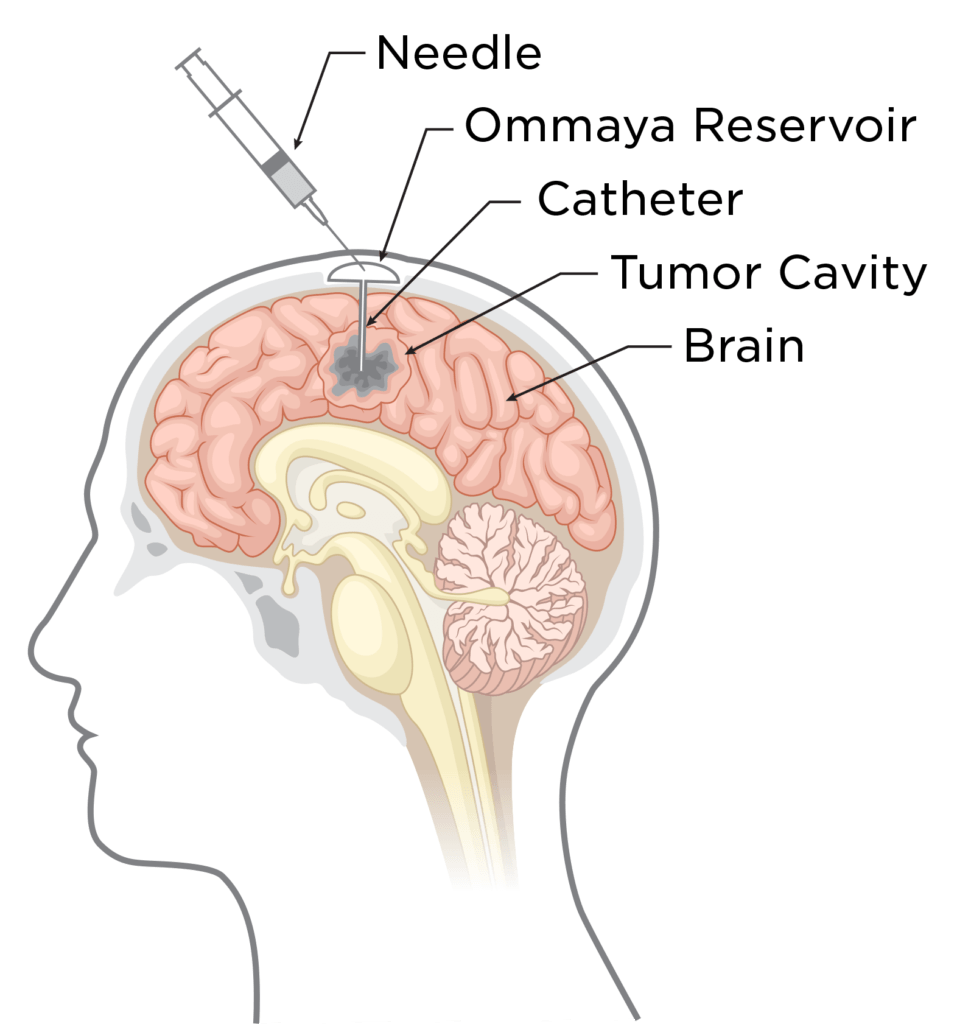
This technique allows neurosurgeons to place a biologically inert reservoir, known as Ommaya, under the scalp at the end of the patient’s resection surgery. The reservoir connects to a small catheter sitting within the tumor resection cavity.
Following surgery, during patients’ routine clinical visits, Ivy Center physicians can quickly access the Ommaya reservoir using a sterile needle to draw a cerebrospinal fluid (CSF) sample. Tumor-specific genetic material (DNA and RNA) from the CSF is then analyzed and compared to prior samples. This allows doctors–and patients–to learn if glioblastoma drugs are working as hoped or whether a different protocol should be followed.
“One of the largest barriers in clinical trials [and treating glioblastoma in general] is the lack of access to brain tumor tissue, which tells us what is happening in real-time,” explains Barrow Neurosurgery Chief Resident Charuta Furey, MD. “This is a minimally invasive way to track and treat patients’ tumors more effectively.”
Dr. Furey explains that while tissue can be collected and analyzed at the time of tumor resection, doctors can now more frequently analyze how a patient’s tumor cells are evolving. Ultimately, this program gives patients greater hope to extend their own lives while helping others in the future have access to the most successful forms of treating glioblastoma.